 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
|
|
|
|
 |
| If you are interested in receiving the
copy of the newsletter, do write to us. Join our nework. Click here>> |
|
|

Ignoring the future
There is substantial resistance among the medical community
and policy makers with regard to accepting the increasing evidence of the impact of these
toxics on human health. Some people believe that NO chemicals in the environment could
possibly cause cancer because humans are exposed to very small quantities. A review by the
National Toxicology Program of the United States Environmental Protection Agency (EPA),
found that just 6 per cent of 216 chemicals tested, increased cancer risk and that too
only at high doses.1 Others
believe that EVERY chemical can cause cancer. Of course, this is also false. In a later
study by the National Toxicology Program, of the 253 chemicals chosen for testing because
of their suspected carcinogenicity, about 70 per cent caused cancer in high-dose animal
studies and more importantly, about 20 per cent of the chemicals were found to be
carcinogenic even at low doses.2 The
truth, therefore, is somewhere in between the two arguments. A significant fraction of
chemicals in the environment, about 10 to 20 per cent, may have the potential to cause
cancer in humans at low doses. Exposure to chemicals is just one environmental factor that
combines with children’s genetic predispositions to cause cancer; others include
diet, smoking habits, alcohol consumption, and exposure to sunlight, radiation, and
viruses.Evidence of absence
| DDT
levels Developed countries have low levels
of DDT in human milk in comparision to developing countries |
 |
| Adapted from: F Ejobi et al 1996,
Organochlorine pesticide residue in mother’s milk in Uganda, Bulletin of
Environmental Contamination and Toxicology, 56:875, New York. |
Diseases, ailments and syndromes that have commonly been
attributed to chemicals are cancers (to dioxins, pesticides and metals), neurological
disorders like Alzheimer’s disease (to aluminium), eczema (to hardness of water) and
diabetes mellitus (to increased nitrates in water). Cancers like bladder cancer and
non-Hodgkin’s lymphoma are strongly associated with the high presence of nitrates in
water.3 A study of children in five
villages in Rajasthan found that high nitrate ingestion in drinking water together with
methemoglobinemia, causes and aggravates recurrent acute respiratory tract infections and
may be the reason for high mortality in children.4
Even "safer" pesticides used in homes have been incriminated to cause
Parkinson’s disease, 5 breast cancer
6 and cognitive dysfunction.7 Risks are often widespread and across
borders. In Turkmenistan, for example, dust is richly laden with hazardous pesticides,
carried from neighbouring countries and regions. This dust contains anywhere between 1.
8 to 126 milligrams of particulate matter per
kilogram of dust deposited per hectare of land. Evidence suggests that there is an
increase in interstitial lung disease in children in the region8. Parental occupation also
poses risks to children 9, 10,11.
Reproductive disorders from endocrine disruptors,
hormonally-related cancers, and infertility also appear to be on the rise. During the past
50 years, the rate of testicular cancer in industrialised countries has increased by a
factor of two to four. Breast cancer mortality in the United States has been rising by
about one per cent per year since the 1940s. There is some evidence that sperm counts and
semen volume may have declined substantially.12
There are also signs that abnormal sexual development in infants may be increasing. A
doubling of the incidence of undescended testes in male infants since 1960 has been
reported in the United Kingdom.13
Today’s increased prevalence of these reproductive problems is puzzling. Some
increases in cancer rates have occurred in the elderly but more disturbingly, these
symptoms have also been observed in younger populations. Most studies on these phenomena
conclude that long-term exposure, initiated in childhood was responsible for these
conditions. However, so far no studies on these issues have been done in India.
Some
people believe that NO chemicals in the environment could possibly cause cancer because
humans are exposed to very small quantities |
…or absence of evidence?
The sudden rise of modern disease epidemics has taken the
Indian medical fraternity by surprise. Physicians in Mumbai, for example, found they were
under-diagnosing asthma. The prevalence was actually 17 per cent, compared with 3.5 per
cent by physician diagnosis.14
Similarly, unexplained rise in the number of cancer patients from areas not considered
"hotspots" for cancers is alarming doctors in India. In Delhi alone, six new
cancer treatment hospitals have sprung up in the past five years. Even the many Government
of India registries show that cancers are on the rise in children (though, shockingly, the
government has not produced a comprehensive report for about a decade!). What is even more
alarming is that the numbers of unexplained causes of child deaths have increased
dramatically.
Pesticides that have long been phased out in developed countries, and banned/restricted
food additives and preservatives are liberally marketed in India. Enforcement agencies
like the Bureau of India Standards, pollution control boards and more importantly the
Ministry of Health and Family Welfare have no synergy or cooperation to deal with these
challenges. Clearly, enforcement and regulatory agencies are keen to adopt best prevailing
standards but are at least a generation behind in implementing them.
| Killer
air… |
| At last there now comes conclusive
evidence that tiny particles in the air increase the risk of human death. A recent study
published in the Journal of American Medical Association, co-authored by C Arden Pope,
professor of economics at the Brigham Young University finds that a mere increase of 10
microgrammes per cubic metre (µg/cu.m) of fine particles (size less than 2.5 microns or
PM2.5) increases the risk of lung cancer by 8 per cent, that of cardiopulmonary deaths by
6 per cent and all deaths by 4 per cent. To really understand how air pollution results in
increased risk for lung cancer, the effect of smoking on lung cancer risk was taken into
account. The study thus help provide new insights into lung cancer risk. The research took place over a period of sixteen years, covering 116
metropolitan areas of United States and covered about 500,000 people. The study is a part
of the ongoing prospective mortality study of approximately 1.2 million adults, the
analysis of which is based on the data collected by the American Cancer Society. "The
findings of this study provide the strongest evidence to date that long-term exposure to
air pollution, common to many metropolitan areas in the US, is an important risk factor
for cardiopulmonary and lung cancer mortality," according to Pope.
The study shows that despite improvements in the falling
rates of fine particulate levels, the levels are still high enough to be associated with a
significantly increased risk of cancer and cardiopulmonary deaths. In 1999-2000, the
annual average particulate air pollution level recorded in New York was 16 µg/cu.m, with
Los Angeles, Chicago and Washington, DC reporting 20 µg/cu.m, 18 µg/cu.m and 15 µg/cu.m
respectively. Compare this to the levels recorded during 1979-1983: New York City 24
µg/cu.m, Los Angeles 27 µg/cu.m, Chicago 23 µg/cu.m and Washington DC 15 µg/cu.m. Yet,
the risks to human health remain high.
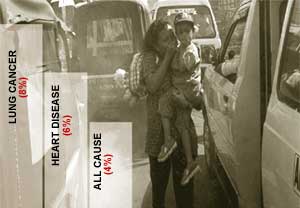 With air
quality levels in most of the Indian cities higher than expected, it is not a surprise to
come across more incidences of respiratory illnesses, breathlessness and reduced lung
function. In Delhi alone, about 7.5-10 per cent of males suffer from various respiratory
diseases. With air
quality levels in most of the Indian cities higher than expected, it is not a surprise to
come across more incidences of respiratory illnesses, breathlessness and reduced lung
function. In Delhi alone, about 7.5-10 per cent of males suffer from various respiratory
diseases.
Clearly, the time has come to ask for our right to clean
air.
|
The concept of environmental health has emerged only in the
past 30 years or so and is yet to receive recognition from medical fraternity. The warning
given in Rachel Carson’s Silent Spring (1962) that pesticides were creating
greater problems than they were intended to solve-started off a controversy still raging
today between environmentalists and the pesticide industry. More evident and large-scale
disasters like Bhopal, Soveso dioxin poisoning, the Minamata mercury poisoning have moved
governments to create effective policy measures and regulatory bodies, but it does not
seem to have deterred industries from producing chemicals or at least conduct studies on
their safety and long term implications. Therefore educating people on the impact of
chemicals and toxics in their daily life is more important and more effective in bringing
about this change. Modern diseases are the driving force of environmental health as a
discipline in the developed countries. But India suffers from a double burden of diseases
which pose more questions and reveals few answers on how they will interact and impact
children. The needs to approach is of integrating health and environment, both in the
research agenda, policy domain and in clinical diagnosis and treatment by medical
practitioners. So far, environmental causes to diseases are not considered in the
"radar" of diagnosis. But there is hope that with increase in awareness, this
mindset will change and there will be more holistic approach to diseases.
References
1-2. National Toxicology Program
Studies available at www.ntp-server.niehs.nih.gov (as on March 12, 2002).
3. Peter Weyer 2001, Nitrate in Drinking Water Increases Bladder Cancer
Risk, FDA Center for Food Safety and Applied Nutrition, Consumer Advisory, April 11, http://www.cfsan.fda.gov/~dms/supplmnt.html.
4. Sunil Kumar Gupta et al 2000, Recurrent acute respiratory tract
infections in areas with high nitrate concentrations in drinking water, Environmental
Health Perspectives, Vol 108, Number 4, April.
5. Joan Stephenson 2001, Exposure to Home pesticides linked to Parkinson
disease, Journal of American Medical Association;283: 23,p 3055; and Alessandra
Menegon et al 1998, Parkinson’s disease, pesticides, and glutathione transferase
polymorphisms, The Lancet, Vol 352, October 24, p 1344.
6. Annette Pernille Høyer et al 1998, Organochlorine exposure and risk of
breast cancer, The Lancet, Vol 352, December 5.
7. H Bosma et al 2000, Pesticide exposure and risk of mild cognitive
dysfunction, The Lancet, Vol 365, September 9.
8. Sarah L O’Hara et al 2000, Exposure to airborne dust contaminated
with pesticide in the Aral Sea region, The Lancet, Vol 355, February 19, p 627.
9. E Tielemans et al 1999, Pesticide exposure and decreased fertilisation
rates in vitro, The Lancet; 354: p 484-85.
10. C Infante-Rivard et al 1991, Risk factors for cancer in the
workplace. Boca Raton, FL: CRC Press.
11. L M Anderson et al 1994, Preconception exposure of males and
neoplasia in their progeny: effect of metals and consideration of mechanisms. in: D R
Mattison, A F Olshan, eds. Male-mediated developmental toxicity. New York: Plenum
Press.
12. E Carlsen et al 1992, Evidence for decreasing quality of sperm of
semen during past 50 years, British Medical Journal; 304:609-613.
13. Anon 1986, The World in Medicine 1986, British Medical Journal;
293:1401-1404.
14. Anon 1998, Editorial, Journal of American Medical Association,
Vol 280, No 10, September 9, p 873. |
|
 Previous | MORE VULNERABLE
1 2 Previous | MORE VULNERABLE
1 2 |
|
|

